Targeting Approaches for Effective Therapeutics of Bone Tuberculosis
Nigar Sultana Shaikh and Sujata P Sawarkar
Nigar Sultana Shaikh and Sujata P Sawarkar*
SVKM’s Dr. Bhanuben Nanavati College of Pharmacy, V. M. Road, Vile Parle (W) Mumbai 400 056, India
- *Corresponding Author:
- Sujata P. Sawarkar
Associate Professor, Department of Pharmaceutics, SVKM’s Dr. Bhanuben Nanavati College of Pharmacy, 1st Floor, Gate No.1, V.M. Road.Vile Parle (West), Mumbai, India
Tel: 91-22-42332052 / 9819186702
E-mail: Sujata.sawarkar@bncp.ac.in
Received Date: April 20, 2016; Accepted Date: December 26, 2016; Published Date: January 07, 2017
Citation: Shaikh NS, Sawarkar SP. Targeting Approaches for Effective Therapeutics of Bone Tuberculosis. J Pharm Microbiol. 2017, 3:1.
Abstract
Bone and Joint Tuberculosis (TB) is the major and commonly occurring type of extra pulmonary mycobacterial disease. Since last twenty years the occurrence of bone TB has augmented marginally in specifically economically backward or developing nations due to malnutrition. Moreover decrease in immunity results in increase in occurrence in patients suffering from AIDS. Bone TB is also found in cases where the organism has developed resistance to the drug treatment of pulmonary TB and when there is propagation of tuberculosis from the affected lungs to the whole body through the blood vessels. Corrective Surgery along with precise antitubercular drug therapy for longer period of time is commonly preferred in subjects where neurological defects are occurring along with bone deformity. This combined treatment has exhibited satisfactory results. The present line of treatment for bone TB includes ATDs administered by oral/ intravenous or intramuscular route coupled along with surgical treatment of incorporating Autogenous bone graft and Titanium Mesh Cage to regenerate the deceased bone. This review focuses on approaches for tackling bone tuberculosis and various vertebrate deformities and treatments by medicinal use and by avoiding the surgical approaches.
Keywords
Bone tuberculosis, Paraplegia; Tuberculous vertebral osteomyelitis, Mycobacterial bone infections; Autogenous Bone Grafts; Titanium mesh cage; Poly-DL- lactide (PDLLA); Nano Hydroxy Appetite (nHA), Mycolic acid targeted ligand; Intraosseous injectable preparation
Introduction
Tuberculosis is a potentially fatal contagious disease and is one of the foremost, infectious disease and one of leading cause of death in the world. About more than 1 million people die every year because of this disease. The bacteria infects predominantly lungs however it can affect any part of the body. It is been known since ancient times that Mycobacterium tuberculosis is also responsible for affecting bones and joints area. It is also called as tuberculosis osteomyelitis or nontuberculous mycobacterial (NTM) skeletal infections.
These infections generally occur due to restoration and revival of infection when mycobacterial gets harboured in the bone when pulmonary infection spreads and reaches to non-pulmonary site i.e. bones during primary infection by mycobacteria [1,2]. The disease is caused by a bacterial microorganism, the tubercles bacillus viz. Mycobacterium tuberculosis, Mycobacterium bovis,Mycobacterium kansasii, Mycobacterium fortuitum, Mycobacterium marinum, or Mycobacterium intracellulare.
Difficulties and prolongation in detection and diagnosis, absence of effective and specific vaccine, long treatment schedules, lack of understanding of methodology that regulate spread of infection, restoration, progression of disease are the major reasons behind failure to control the spread of TB. The vaccination with Mycobacterium bovis bacillus Calmette Guerin (BCG) has been effective in providing protection and preventing in mortality in some cases however in some cases the vaccination has been ineffective and inadequate in controlling the disease.
A new way to determine that whether the individuals have been infected or not is by Mycobacterium tuberculosis antigen-specific interferon gamma (IFN-c) release assays, but they cannot distinguish that which individuals are infected with active tuberculosis and which are with latently Mycobacterium tuberculosis.
The occurrence of osteoarticular disease is seen after the principal lesions of lungs spreads phenomenally via lymph nodes, secondarily to when there is involvement of lymph node and along with visceral lesions, there are concurrent presence of renal and hepatic tuberculosis especially seen in diabetic patients. The presence of skeletal TB is comparable to that found in non HIV patients. The commonly occurring type of skeletal TB involves spine and termed as Pott’s disease. This disease occurs in 50% cases of musculoskeletal TB. The commonly occurring musculoskeletal TB is Tuberculosis arthritis and extra spinal tuberculosis osteomyelitis.
The reason as to why bacilli get transmitted to spine and large joints is because of rich perfusion or vascular supply to the vertebra and growth plates of the long bones. Tuberculosis arthritis can also occur because of spread of initial infection to the bone and joint. Tuberculosis bacilli exhibit the tendency of migrating from the lung to the spine via Batson paravertebral venous plexus or by lymphatic drainage to the Para aortic lymph nodes and hence infecting the bones and joints and hence infecting the bones and joints. Another cause of infection is direct inoculation by of mycobacteria following a traumatic injury or during surgical procedures like joint arthroplasty. In case of patients where immunity and resistance is compromised for example, HIV-AIDS and organ transplant recipients, the infection can be caused by propagation through blood. The direct seeding of bacteria after a traumatic injury like joint arthroplasty causes secondary problems involving NTM osteoarticular infections. Immune compromised patients are at higher risk of Haematogenous dissemination and NTM bone infections. In some cases, the bacteria Mycobacterium bovis reaches vertebral column from urinary bladder via the route of Batson venous plexus Osteoarticular tuberculosis is widespread extra pulmonary TB affecting spine, joints, feet, upper extremity and elbow. Although sometimes pulmonary TB spreads to bones and joints. The disease leads to extensive pain, arthritis, paralysis, obliteration of the vertebrae and discs resulting in spinal hump. The occurrence of pain in case of bone TB is often wrongly diagnosed as frozen shoulder.
Types of Bone Tuberculosis [3,4]
Tuberculosis of spine
This is the most common type of bone TB occurring in about 50% cases. Vertebral and skeletal lesion is commonly diagnosed in these cases. In recent times the number of cases in India with TB of spine has increased from 30,000 to 90,000 Tuberculosis of sacro-iliac joint: TB at this site is often not detected. Tenderness is commonly observed in the affected region. Lesions are seen in sacral and iliac region and abscess is often seen either intra pelvic or under the glutei Maximus muscle. This type of TB can be diagnosed either by removal of pus from the lesion or by needle biopsy. This type of TB can be treated by anti-tubercular drugs and protective bracing.
Tuberculosis of hip joint
Hip joint TB is next common TB after spine TB. It occurs in all the age groups but commonly seen in malnourished children.
Tuberculosis of knee joint
This type of TB is seen in patients of all age groups. The common symptoms in patients are pain during the movement of knee joint, secretions from synovial region, conspicuous thickening at the synovial joint and tenderness leading to dislocation of knee, dislodgment of lateral, posterior and superior tibia on femur.
Tuberculosis of ankle joint
Lesions associated with this type of TB are commonly observed in tibia, fibula and talus region. Clinical symptoms are similar to the other previous types of bone TBs. Osteochondritis desicans of talus also shows similar symptoms as this type of TB. Tuberculosis of foot: Tubercular Lesions in the foot can be isolated in certain regions leading to talocalcaneal arthritis and peroneal spastic flat foot.
Tuberculosis of upper extremity
In this kind of TB, shoulders are affected. This disease is commonly seen in adults. The affected sites of shoulders are head of humerus, glenoid, spine of the scapula, acro- mio-clavicular joint, coracoid process and synovial lesion. This therapeutic condition is often wrongly diagnosed as frozen shoulder in diabetic patients and physicians often wrongly treat the patients with iatrogenic steroid injection.
Tuberculosis of elbow
The affected portions of elbow are medial and lateral condyles of the humerus, articular surface of olecranon-intra articular (rarely extra articular) and head of radius. Thickening of radiohumeral segment of synovium is observed. This deformity can be easily detected during x ray examination which is indicative of the presence of the infection (Figure 1).
Patients with Bone TB may or may not show classic symptoms of pulmonary TB like fever, exhaustion, weakness, night sweats and unexplained weight loss, extensive cough, congested pulmonary system.
Symptoms of Bone Tuberculosis
Pain
Tuberculosis most commonly attacks the spinal region and at the joints which bear the weight of the body. Depending on the location of Tuberculosis, location of the pain varies. TB in the joints often results acute pain and stiffness. Spinal tuberculosis is also termed as Pott’s disease which usually affects thoracic region of the spine. As the mycobacteria affect the disc cushioning the vertebra, patients constantly suffer from back pain. Tuberculosis osteomyelitis causes constant pain in the bone itself and leading to complications in nearby tissues, such as carpal tunnel syndrome if the wrist is affected.
Arthritis
Tuberculosis of the joints is also called articular TB. This type of TB badly affects the joints of the hips and knees. As a result the stiffness and abscesses is developed in the affected joints.
Paralysis
Spinal tuberculosis if not diagnosed and mitigated on time can rapidly affect the entire vertebral column. As a result of this spinal column can destroy leading to paralysis of the lower section of the body.
Spinal hump
Advancement of spinal TB leads to destruction of vertebrae, discs. As a result, bones of the spine protrude forward. The treating physician diagnoses by feeling the dislodging of the bones of the spine to form a hump called as gibbous. Patients with bone TB may or may not show classic symptoms of TB such as fever, night sweats, and weight loss. However 50% of the patients of bone TB also have infected lungs. However in the lungs region, the infection is dormant. Patients suffering from bone TB are not contagious as this disease spreads by coughing up of mycobacterial particles.
Epidemiology
Osteoarticular tuberculosis, is found in about 10%-20% of all diagnosed tuberculosis, is the most common extra pulmonary tuberculosis The epidemiology of Bone and joint TB accounts for 2.2-4.7% of all TB cases in Europe and the USA and around 10-15% of extra pulmonary tuberculosis (EPTB) cases, whereas in undeveloped countries, particularly Asia, the incidence of EPTB increases to 15-20%. In developed countries, 58-81% of skeletal TB cases are diagnosed in immigrants, and in the USA, 10% of EPTB cases occur in HIV-infected patients [5-8].
Clinical Features
The current studies states that the average age of patients suffering with tuberculosis vertebral osteomyelitis belongs to the age group of 45-60 years [9]. However studies indicate that patients of age between 20-30 years get infected due to immigration and HIV infection and in patients of age between 60- 70 years. The incidence of concomitant extra spinal involvement varies (5-50%) and concomitant lung disease is observed in more than 50% cases [10]. Onset of symptoms, development and progression of disease in spinal TB is usually a very slow process. The time required to diagnosis the symptoms ranges from 2 weeks to several years. Back pain is usually present in 83%, but only onethird of patients have fever or constitutional symptoms. All these are more frequent in patients with associated extra spinal TB and those with disseminated disease [11]. Tuberculosis vertebral osteomyelitis affects the thoracic or thoracic-lumbar segment in around half of the cases, followed by the lumbar segment, and to a much lesser extent, the cervical segment. Multifocal noncontiguous spinal involvement is reported to be uncommon in some studies, but is observed in 16.3-71.4% of cases when wholebody MRI is performed. Non-contiguous spinal TB is common in areas that have a high prevalence of mycobacterial infection as indicated in Table 1. The prevalence of the disease is around 30 million globally and approximately 30% or 10 million cases exist in India, 1-3% of the 10 million have involvement of bones & joints. The predisposing factors are malnutrition of the protein calorie type, environmental conditions and living standards such as poor sanitation, overcrowded housing and slum dwelling. Repeated pregnancies and lactation in women is also a factor. A diabetic status is an important pre-disposing factor. Acquired immune deficiency syndrome has certainly led to a resurgence of tuberculosis [12]. The onset of symptoms is usually slow in spinal TB and then progression to disease is a very long process, but an acute onset has also been reported. The duration of diagnosis ranges from 2 weeks to several years. Earlier the average time taken to diagnose the disease was at least 12 months, but more recent publications report symptom duration of 2-7 months. Back pain is usually present (83-100%), but only one-third of patients have fever or constitutional symptoms. These manifestations are more frequent in patients with associated extra spinal TB and those with disseminated disease.
| Country (Year) | No. of cases | Incidence of all TB (%) | % of EPTBpatients |
% Immigrants |
Concomitant pulmonary TB (%) | Spine involvement (%) |
|---|---|---|---|---|---|---|
| Denmark (2000) | 95 | 4 | 15 | 2/3 | - | 50 |
| Netherlands(2004) | 532 | 4.3 | 10.6 | 58 | 29 | 56 |
| England-W (1984) | 198 | 4.7 | - | 60 | 15 | 36 |
| USA (2009) | 5337 | 2.2 | 11.3 | 81 | 6.9 | - |
| Turkey (2011) | 11 | 2.7 | 11 | - | - | - |
| Spain(2007) | 53 | - | - | 15 | 15 | 64 |
Table 1 Epidemiology of EPTB in developed countries [12].
Areas most affected by tuberculosis vertebral osteomyelitis are thoracic or thoraco-lumbar segment in half of the cases, followed by the lumbar segment, and to a much lesser extent, the cervical segment. When whole-body MRI is performed multifocal noncontiguous spinal involvement is reported in 16.3-71.4% of cases. Non-contiguous spinal TB is common in areas that have a high prevalence of mycobacterium infection, such as South Africa. There is occurrence of some neurological complications in approximately 50% of spinal TB patients due to compression of the spinal cord or other nerve roots. In patients with cervical or thoracic spinal TB chances of development of paraplegia or tetraplegia is around 40-50%. Neurological complications are more common in patients with associated epidural abscess [13-15].
Pathogenesis and Pathology
At the stage of primary M. Tuberculosis infection, bacillemia may lead to seeding of microorganisms in bone/synovial tissue. In majority of cases small foci of infection are restricted to small region because of local adaptive immune processes and as result the infection remains restricted and subclinical, localized at one place. However in cases of malnutrition, advancing age , HIV infection, renal failure, when immune responses fail, the primary infection which is localized and focussed at one place gets activated and if not treated with timely diligence the spinal segments (vertebrae) may collapse and cause paralysis in one or both legs [16,17]. Multi-level non-contiguous vertebral tuberculosis is another atypical form of spinal tuberculosis wherein two non-contiguous vertebrae are affected without causing any destruction of the adjacent vertebral bodies and intervertebral disks. The patients affected have been found to be asymptomatic. In this retrospective analysis, those patients were included whose spinal infection was identified by whole spine magnetic resonance imaging (MRI) and had been confirmed as tuberculosis by a combination of histology and microbiology [18]. The most devastating complication of spinal tuberculosis is Paraplegia. Paraplegia is classified into two groups according to the activity of the tuberculosis infection. These two groups are paraplegia of active disease (early-onset paraplegia) called as Pott’s spine and paraplegia of healed disease (late-onset paraplegia). The causes of paraplegia are depicted in Table 2 [19].
| Early-onset paraplegia | |
|---|---|
| Spinal artery thrombosis | Infective thrombosis of anterior spinal artery |
| Mechanical pressure | Mechanical pressure by tuberculous debris, sequestrem of bone or disk, abscess, subluxation and dislocations, concertina collapse, and internal gibbus |
| Tuberculousgranuloma | Tuberculoma in extradural, intradural, or intramedullary regions |
| Tuberculous myelitis | Uncommon. May involve spinal cord parenchyma |
| Transection of spinal cord by bony bridge | Transverse ridge of bone produced by severe kyphosis |
| Fibrosis of dura (pachymeningitis) | Formation of tough, fibrous membrane encircling the cord |
Table 2 Mechanisms of paraplegia/tetraplegia in spinal tuberculosis.
Commonly used Drugs for the Treatment [19-22]
First line drug for the treatment of bone tuberculosis are Isoniazid (INH), Rifampicin (RIF), Pyrazinamide (PZA), Streptomycin (SM) and Ethambutol (EMB), which are given for six months. It has been observed that Isoniazid frequently develops resistance and hence initial treatments includes a combination of five drugs viz. Isoniazid, Rifampicin, Pyrazinamide, Streptomycin and Ethambutol. Rifampicin and Pyrazinamide are the most effective sterilizing drugs, and they are specifically effective against bacilli that are dormant and undergo periodic bursts of activity. Table 3 indicates the target sites of the active therapeutic drugs and the genes involved in developing resistance of the drugs. The most common adverse reaction associated is gastrointestinal upset, mild jaundice. Pyrazinamide is also another bactericidal for Mycobacterium tuberculosis. In case of failure of treatment with first line drugs due to development of bacterial drug resistance, second-line drugs such as Para-amino salicylates (PAS), Kanamycin, Fluor quinolones, Capreomycin, Ethionamide and Cycloserin are employed. The treatment is commenced with initial first line drugs for period of two months as a result the bacteria gets destroyed at growth stages, after which the treatment is continued with RIF and INH singly for up to four months. In case if there are remnant dormant bacilli they get eradicated by RIF and if there are any remaining RIF resistant mutants left they are killed by INH. Resistance to a single anti-TB drug is a common phenomenon seen in most of the cases.
| Drugs | MIC (µg/ml) |
Mechanisms of Action | Target | Genes involved in Resistance | ||
|---|---|---|---|---|---|---|
| Isoniazid | 0.01-0.20 | Inhibition of cell wall mycolic acid sunthesis | Enoyl acyl carrier protein reductase (InhA) | KatG, InhA | ||
| Rifampicin | 0.05-0.50 | Inhibition synthesis | of | RNA | RNA polymerase,β subunit | rpoB |
| Pyrazinamide | 20-100 | Depletion of membrane energy | Membrane energy metabolism | pncA | ||
| Ethambutol | 1-5 | Inhibition of cell wall arabinogalactam synthesis | Arabinosyltransferase | embCAB | ||
| Streptomycin | 2-8 | Inhibition synthesis | of | protein | Ribosomal S12 protein | rpsL, rrs |
| Kanamycin | 1-8 | Inhibition synthesis | of | protein | 16S Rrna | Rrs |
| Capreomycin | 4 | Inhibition synthesis | of | protein | 16S rRNA,50S ribosomes, rRNAmethyltransferase(TlyA) |
RrstlyA |
Table 3. Current Anti-Tb drugs and their targets [21,22].
Multi-Drug resistant tuberculosis (MDR-TB) therapy duration can extend up to two years. Ideal therapy should include less toxic, active and less expensive drugs, usually involving any first-line drugs to which the strain is still susceptible and alternative or second-line drugs [23].
Rifampicin (RIF), one of the first-line anti-TB drugs, has been structurally modified to newer drugs viz. rifalazil, rifalutin and rifapentine. These agents can be given once or twice weekly, instead of daily RIF dosing due to their longer half-lives and increased in vitro potency [24].
Older agents such as ethionamide, capreomycin and paraaminosalicylic acid can be used, as well as newer classes, generation of drugs, such as fluoroquinolones (ofloxacin, moxifloxacin), penicillin/ β-lactamase inhibitors and other members of the rifampicin class (rifabutin, rifapentine) can also be selected.
The WHO recommended DOTS (directly observed treatment, short course) anti-TB therapy which involves four drugs; Isoniazid, rifampin, pyrazinamide and ethambutol or streptomycin. WHO has recommended the Fixed dose combination (FDC) of Rifampicin (RIF), Isoniazid (INH) and Pyrazinamide (PYZ) or PYZ with Ethambutol (ETB). The details of marketed formulations of First Line and Second line drugs available, their dose, aqueous solubility and their Bio pharmaceutics Classification (BCS) [25] are given in Table 4.
First Line drugs
| Drug | Brand Name | Dose (mg) | Aqueous Solubility (mg/mL) | BCS Class |
|---|---|---|---|---|
| Isoniazid | Nydrazid | 300 | 125 | III |
| Rifampicin | Rifadin | 300 | 1-2 | II/IV |
| Pyrazinamide | Zinamide | 500 | 14 | III |
| Ethambutolhydrochloride | Myambutol | 400 | 100 | III |
| Streptomycin | Sesquisulfate- AgriStrep | 500 | >20 | IM/IV |
| Rifabutin | Mycobutin | 150 | 0.19 | II |
Second line drugs
| Drug | Brand Name | Dose (mg) | Aqueous Solubility (mg/mL) | BCSClass |
|---|---|---|---|---|
| Clofazimine | Lamprene | 100 | 0.01 | II |
| Ethionamide | Trecator; Ethimide | 500 | 0.1 | II |
| Clarithromycin | Biaxin | 500 | 0.00033 | II |
| p-Aminosalicylic acid | Rezipas | 500 | 1.7 | - |
| Cycloserine | Oxamycin | 500 | 100 | IV/II |
| Amikacin | Amiklin, Novamin | 1000 | - | III |
| Kanamycin A | Kantrex | 1000 | - | iv/im |
| Fluoroquinoloneslike Levofloxacin, | Avelox- Moxifloxacin | 400 | - | Oral /iv |
| Gatifloxacin&Moxifloxacin | ||||
| Levaquin-Levofloxacin | 500 | Sparingly soluble | IV | |
| Kyorin - Gatifloxacin | 400 | 60mg/mL | - | |
| Linezolid | Zyvox, Zyvoxid | 400 | Soluble in water up to 3 mg/mL | - |
Table 4. Details of marketed brands of First line and Second line Drugs and their BCS class.
Most of the drugs used for the treatment of TB belong to BCS II or IV. It is because of their compromised solubility or permeability resulting into poor bioavailability, they are either administered in high doses by oral route or by intramuscular / intravenous route. The therapy is for prolonged duration with extensive consumption of high dose pills. This results in low patient compliance and adherence to treatment schedules and therapeutic failure leading to multidrug resistance. Effective implementation of DOTS has been difficult, especially in developing countries and rural areas. The major problem associated with anti-tubercular drugs (ATDs) is limited and erratic bioavailability. Many of the times, TB and HIV conditions coexist. In these clinical circumstances absorption rates are severely affected and intestinal malabsorption of ATDs is observed after oral administration. RIF, the commonly used drug shows erratic bioavailability. The drug displays a strong pH-dependent solubility wherein the drug shows low aqueous solubility and good absorption in the stomach.
The drug undergoes hydrolysis to poorly soluble forms such as 3-formyl Rifampicin SV and 1-amino-4-methyl piperazine under acid gastric conditions. At intestinal pH-values it undergoes oxidation to an insoluble Quinone derivative or a desacetylated form.
In case of FDC, presence of INH hampers the absorption of RIF due to the reaction between both drugs in the gastric medium to form an insoluble hydrazine. The drug RIF shows interaction with food, and other drugs.
Some of the newer drugs which are various stages of clinical trials include SQ109 (Etambutol analogue with adamantly ring - Sequels Inc.), PA-824 (bicyclic nitroimidazo[2,1-b]oxazines- TB Alliance and Novartis), OPC-67683 (6-nitro-2,3-dihydroimidazo[2,1-b] oxazoles - Otsuka), TMC207 (diarylquinolines- Johnson and Johnson) , LL-3858 (Sudoterb®- Lupine), FAS 20013 (FASgen, Inc) [26,27].
The most common side effects associated with most common anti-tubercular drugs are depicted in Table 5. As evident from the above examples these drugs since they are administered in high doses, they exhibit prominent side effects like nausea, vomiting etc. The side effects associated with commonly used drugs are severe hepatotoxicity caused by RIF, deafness or vestibular functional derangement caused by Streptomycin, depressed thyroid function caused by Ethambutol [28-30]. Extensive treatment with these drugs causes microorganisms to develop resistance. In case of resistance to first line therapy clinicians resort to second line drugs. Sometimes, these second-line drugs are found to be more toxic and less clinically active than first-line agents.
| Drug | Major adverse effects | Rare adverse effects |
|---|---|---|
| Isoniazid | Peripheral neuropathy, skin rash, hepatitis, sleepinessandlethargy | Convulsions, psychosis, arthralgia, anemia |
| Rifampin | Gastrointestinal abdominal pain, nausea, vomiting,hepatitis,generalizedcutaneous | Osteomalacia, pseudo-membranous colitis, pseudo-adrenalcrisis,severerenalstoppage, hemolyticbloodpaucity |
| Pyrazinamide | Arthralgia, hepatitis, gastrointestinal problems, eg, stomach upset, nausea, poor appetite and abdominal pain | Cutaneous reaction, sideroblastic anemia |
| Streptomycin | Vestibular and auditory nerve damage renal breakage, cutaneous allergic reaction | Pain,rashatinjectionsite,numbnessaround the mouth and tingling soon after the injection |
Table 5. Side effects of Antitubercular drugs.
Resistance Issues with Conventional Therapy of Tuberculosis [30-32]
1. Multi Drug Resistance Tuberculosis (MDR-TB)
Combination of first line drugs often results in development of resistance. The mycobacteria develop resistance to this combination drug therapy by altering its physiological cycles of RNA synthesis, cell wall synthesis and protein synthesis.
2. Extensively Drug Resistant Tuberculosis (XDR-TB)
XDR-TB, is the abbreviation of the term extensively drug-resistant tuberculosis are cases of TB disease in which patients whose M. tuberculosis clinical isolates / strains were resistant to isoniazid and rifampin and some of the second-line drugs (aminoglycosides, polypeptides, thiazides and Para amino salicylic acid (PAS).
Also it is very hard for the anti-TB drugs to reach the lesion in bone tissue via oral administration. In contrast, liver and kidney dysfunctions are very common in patients who have history of long-term anti-TB drug use.
Hence to deal with the above stated problems, newer molecules and formulation are needed to be developed. Surgical procedure should be restricted to joints with severe cartilage destruction, large abscesses, joint deformity, multiple drug resistance or atypical mycobacteria. Tuberculosis arthritis includes bone marrow oedema, cortical erosion, synovitis, joint effusion, tenosynovitis, soft tissue collection and myositis.
Other issues associated with conventional therapy
ATD drugs are administered either as conventional tablets or as parenteral by intramuscular route and in extreme cases by intravenous infusion.
The major problem associated with anti-tubercular drugs (ATDs) is limited and erratic bioavailability. Many of the times, TB and HIV conditions coexist. In these clinical circumstances absorption rates are severely affected and intestinal malabsorption of ATDs is observed after oral administration.
RIF, the commonly used drug shows erratic bioavailability. The drug displays a strong pH- dependent solubility wherein the drug shows low aqueous solubility and good absorption in the stomach.
The drug undergoes hydrolysis to poorly soluble forms such as 3-formyl Rifampicin SV and 1-amino-4-methyl piperazine under acid gastric conditions. At intestinal pH-values it undergoes oxidation to an insoluble Quinone derivative or a desacetylated form.
In case of FDC, presence of INH hampers the absorption of RIF due to the reaction between both drugs in the gastric medium to form an insoluble hydrazine. The drug RIF shows interaction with food, and other drugs.
As evident from the above examples these drugs since they are administered in high doses, they exhibit prominent side effects like nausea, vomiting etc. The side effects associated with commonly used drugs are severe hepatotoxicity caused by RIF, deafness or vestibular functional derangement caused by Streptomycin, depressed thyroid function caused by Ethambutol [33]. And also extensive treatment with these drugs causes microorganisms to develop resistance. In case of resistance to first line therapy clinicians resort to second line drugs. Sometimes, these secondline drugs are found to be more toxic and less clinically active than first-line agents.
Bone tuberculosis is difficult to treat. Presently osteoarticular TB is treated using standard regimen of ATDs for extensive 8 and 20 months [34]. If oral treatment with ATD does not give encouraging results for mitigation of TB, delivery by intravenous or intraossueus route is adopted. Apart from this measures are taken to resurrect the bone by surgical treatments.
Surgical Treatments
Autogenous bone grafts
Autogenous bone grafts are being considered as standard for bone reconstruction and regeneration however there are many problems associated with it. At times it becomes very difficult to obtain sufficient quantity of autogenous bone tissue in practice. Pain associated with the graft and infections likely to be transmitted from the donor are some of the drawbacks associated with this therapy. In addition there are high chances of occurrence of rejection of graft which is triggered by the immunogenicity of allogeneic bone generally has the ability to regenerate completely provided that a very small fracture space or some sort of scaffold or support is available. Bone grafts may be autologous (bone harvested from the patient’s own body, often from the iliac crest), Figure 2 [35], allograft (cadaveric bone usually obtained from a bone bank), or synthetic (often made of hydroxyapatite or other naturally occurring and biocompatible substances) with similar mechanical properties to bone. The bone grafts are expected to be reabsorbed and replaced as the natural bone rejuvenates and the wound gets healed over a period of time. The mechanism involved in successful bone grafts involve osteo conduction (guiding the reparative growth of the natural bone), osteoinduction (encouraging undifferentiated cells to become active osteoblasts), and osteogenesis (living bone cells in the graft material contribute to bone remodelling) [36,37].
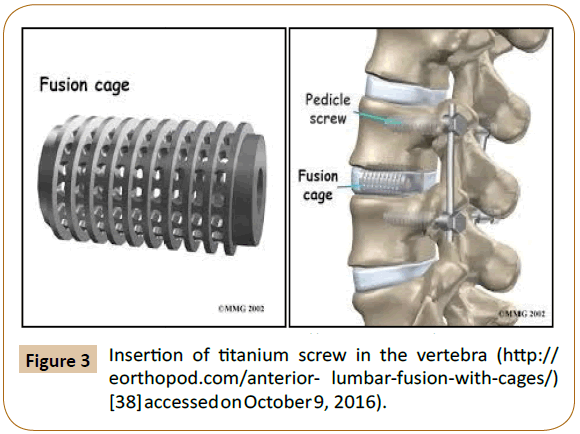
Titanium mesh cage
It has been shown that titanium cage surgery can give good clinical efficacy for spinal reconstruction and stabilisation. Another study demonstrated that a patient with thoracic vertebral tuberculosis satisfactory recovery with no complications when being treated using an antibiotic crescent-shaped polymethylmethacrylate (PMMA) structure for spinal reconstruction and fusion. But titanium mesh and PMMA are not ideal biomaterials to replace autogenous bone as it does not get integrated with the bone tissues. Although titanium mesh could provide some good mechanical support strength, Figure 3 [38], it lacks both osteoconductive and osteoinductive properties [39,40]. The inter-surface of titanium and vertebral body are mechanically combined and because of this loosening occurs with the titanium mesh which further leads to the corrected kyphosis as angle deformation occurs when reconstructing with the titanium cage is done. PMMA exhibits the effect releasing heat during the cure time and thereby enabling healing of damage of the surrounding tissues.
Figure 3: Insertion of titanium screw in the vertebra (https:// eorthopod.com/anterior- lumbar-fusion-with-cages/) [38] accessed on October 9, 2016).
The PMMA monomer cytotoxicity inhibits local macrophage's phagocytic and bactericidal effect. The adverse reactions associated with PMMA are transient decrease/elevation of blood pressure, and even sudden cardiac arrest. During operation it is required to be handled with due diligence otherwise it would cause iatrogenic paraplegia as a result of spinal cord or nerve compression. Therefore, there is an immediate necessity to develop a novel reconstructing / restructuring biomaterial for spinal TB to resolve the problems associated with these treatments [41,42].
Other Approaches of Bone Targeting
Constituents involved in vital aspects of bacterial growth, metabolism and viability, whose inactivation will lead to bacterial death or inability to persist. These should be the desirable targets or darts to knock off the mycobacterial infection. The availability of the Mycobacterium tuberculosis genome sequence and mycobacterial genetic tools, such as transposon mutagenesis, gene transfer, greatly facilitate target identification. Moreover target involved in the pathogenesis of the disease process should also be considered for development of drug as well its carrier. It implies that susceptible target should be correctly identified so that the drug and the carrier developed yield effective and successful therapy. If liquefaction and cavity formation could be interrupted, the bacilli in the lesion would not be coughed up and spread to other organs and tissues.
It has been reported that several bone diseases like osteonecrosis and osteoporosis manifest in local inflammation leading to the incidence of hydroxyapatite in blood [43]. The exposure of hydroxyapatite to blood leads to several possibilities options introduces unique targeting possibilities. Various targeting moieties like tetracycline, Bisphosphonate, acidic oligopeptides, chelating compounds, and salivary proteins have been investigated for bone targeting. Hydroxyapatite is the major component of bone structure. Tetracycline a broadspectrum antibiotic synthesized by Streptomyces genus has been proven in clinical studies that it is taken up by bones due to chemical interaction between Tetracycline and hydroxyapatite Ca10(PO4)6(OH)2, the major constituent of bone tissue [44]. This attribute of Tetracycline binding has been investigated for bone targeting.
Aspartic acid a nonessential amino acid has affinity for hydroxyapatite. Similarly bisphosphonate like Alendronate is taken up by bones [45].
Similarly some of the salivary proteins like statherin and a group of acidic proline-rich phosphoproteins get adsorbed strongly to hydroxyapatite [46].
Some of the polymers conjugated with targeting moieties that have been envisaged in the formulation of carriers or scaffolds for treatment or rejuvenating the bones are as follows:
Poly-DL-lactide (PDLLA)
Poly-DL-lactide (PDLLA) available in an amorphous form has low intensity and gets degrades rapidly. The average degradation time of PDLLA is approximately 12 - 18 months and in vivo the mechanical strength of PDLLA has been found to last for 3 - 6 months, which is beneficial for maintaining the early fixation of bone at the required site and non-weight-bearing area for bone repair. The surface modified three-dimensional (3D) chitosan/PDLLA scaffolds shown histological results as there was significantly higher bone formation potential and better biocompatibility than pure porous PDLLA scaffold in a rabbit radialis defect model in vivo. After being implanted in vivo, the osteocalcin production in the modified PDLLA/chitosan scaffold group was significantly higher (p<0.05) than in the control group. In order to improve the bone repair performance, PDLLA was also added in order to adjust the mechanical properties for other bone repair scaffolds [47,48].
PDLLA exhibited many good attributes for bone repair, still many deficiencies are there that should be improved, such as negative effect on cell growth caused by the acidic degradation products, poor cell adhesion ability caused by the insufficient hydrophilic capacity, maintenance of only short-term mechanical strength and the inconformity of degradation speed with bone repair [49].
In addition to PDLLA, Tetracycline (Tc) grafted PLGA [poly (lacticco-glycolic acid) (PLGA) copolymers] nanoparticles as carriers for bone targeting. Wang et al developed Tc-PLGA nanoparticles for delivery of Simvastatin for the treatment of osteoporosis. Conjugation of Tc to PGA copolymer enhanced the bone targeting ability of the nanoparticles [50]. These nanoparticles can be potentially attempted for accomplishing targeted bone TB therapy.
Yin et al investigated the bone targeting potential of aspartic acid conjugated PLGA-PEG nanoparticles by in vitro using hydroxyapatite assay and in vivo bone affinity assays in
Zebra fish and rats compared it with PLGA-PEG nanoparticles without aspartic acid. The results indicated aspartic acid containing PLGA- PEG nanoparticles showed increased targeting efficiency than PLGA- PEG nanoparticles [51].
Nano Hydroxy Appetite (nHA)
Hydroxyapatite (HA) is the major component of enamel; it gives a manifestation of bright white appearance and removes the diffuse reflectivity of light by closing the small pores / holes of the enamel surface. Because of its excellent biocompatibility, good bioactivity, good torsional modulus, good tensile modulus, tensile strength, and its fatigue resistant effect, it has been proven that the artificial nHA can be considered as the most promising artificial tooth and bone substitute material. Hydroxyapatite has long been among the most studied biomaterials in the medical field for both its proven biocompatibility and for being the main constituent of the mineral part of bone and teeth. Hydroxyapatite is also an important source of calcium and phosphate and is very much important for the remineralisation of demineralized enamel areas. In fact the inorganic component of all the mineralized tissues of the human body is made up of a large prevalence of calcium phosphate salts. Other inorganic materials such as calcium carbonates and sulphates are present in smaller quantities too; in particular hydroxyapatite represents 60-70% and 90% in weight of bone and enamel respectively. Although it has small size, but nHA possesses high solubility, large specific surface area and surface energy. It can chemically bond with natural bone to enhance bone healing very easily. But the disadvantages related to nHA are that, it cannot be individually used as an ideal bone substitute owing to its insufficient mechanical strength and impact toughness. The mechanism used by nHA to exert its effect is diffusion [52]. In vivo when the drug and the materials were loaded, the body fluids get infiltrated into the porous scaffold to dissolve drugs. The drug then diffused from areas of high concentration to the lower concentration environment because of drug concentration differences. The release speed was determined by pore size, porosity and additive components. The external microwave or ultrasound could also have been used to adjust the delivery ratio and release speed in the experiment [53].
Many nHA composites have been successfully fabricated for tissue engineering scaffolds, such as nHA/collagen/poly (vinyl alcohol) composites, nHA/polycaprolactone composites, and nHA/collagen composites. The layer structure of chitosan/nHA composites prepared via in situ hybridization had principally met the bone substitute materials needs for mechanical properties. The flexural strength is up to 86 MPa, which is nearly 3 - 4 times higher than cancellous bone and is equivalent to half of compact bone. The scaffold composed of biodegradable poly diphenyl alanine ethyl ester phosphazene and 100 nm nHA has also shown excellent bone repair ability. The range of hole size is 86 - 145 nm, which is suitable for adsorption and proliferation for osteoblast cells. The compression modulus range is 46 - 81 MPa, which was similar to natural bone [54].
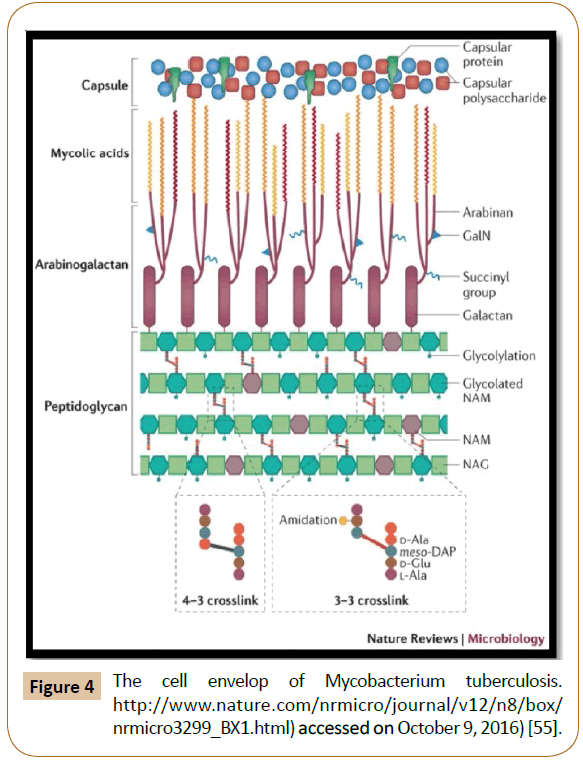
My colic acid targeted ligand
The cell wall of mycobacteria comprises of many chemical components that could serve or behave as targeting ligands. Among these, my colic acids (MA) are promising potential candidates because they are the predominant lipids found in the outer cell wall envelope of Mycobacterium species. MA are long 2-alkyl 3-hydroxyl fatty acids, MA comprise mainly of alpha-, ketoand methoxy classes, typically 70-90 carbon atoms in length, each containing mixtures of homologs of varying chain lengths and, in some cases different stereochemistry around functional groups in the main chain [55,56].
The various subtypes of MA have exhibited a major role and activity responsible for the virulence of the pathogen. MA derived from Mtb have interesting and varied biological activities, including foam cell formation and immune steering towards Th1 cellular responses as well as cholesteroid like properties. MA was also shown to be immunogenic. When presented by CD1b molecules on dendritic cells, proliferation of human CD4−, CD8− (double negative) T-lymphocytes occurs. In addition, anti-MA antibodies are found in human TB-positive patient serum. MA could also target cholesterol present in the plasma membrane of uninfected or infected macrophages and in the membrane of phagosomes in which pathogenic mycobacteria are harboured, by means of its attraction to cholesterol (Figure 4) [57-59]. Presence of My colic acid (MA) in the Nano carriers as ligand has improved the targeting of dosage formulation. In one study Y., Lemmer et al, incorporated Mycolic acid (MA) which is actually a component of mycobacterial cell wall in to the PLGA nanoparticles of INH. The nanoparticles were prepared using double emulsion solvent evaporation freeze drying technique. The microspheres were evaluated for drug encapsulation efficiency, particle size distribution, polydispersity index and zeta potential Presence of MA in the nanoparticles was confirmed by the Enzyme-linked immunosorbent assay (ELISA).
Figure 4: The cell envelop of Mycobacterium tuberculosis. https://www.nature.com/nrmicro/journal/v12/n8/box/ nrmicro3299_BX1.html) accessed on October 9, 2016) [55].
Bone marrow cells were isolated from femurs of female mice and were seeded on tissue culture dishes. After incubation period, the cultured macrophages were infected with mycobacterium species viz. bovis / avium and further incubated in medium devoid of antibiotics. After active replication of mycobacteria for 6 days, infected cells were exposed to INH-encapsulated PLGA NPs medium), with or without the targeting ligand, MA. It was observed that inclusion of MA in the nanoparticles enhanced their phagocytic uptake and therefore enhanced the targeting capacity of developed formulation [60].
Many research and review articles mention the about the colloidal carriers either in form of liposomes, micro or nanoparticles for pulmonary drug delivery for treatment of tuberculosis [61-63].
Scaffolds Yuan et al developed Reinforced β-tricalcium phosphate (β-TCP) scaffolds comprising of Rifampicin where in the drug was loaded by three different solution adsorption methods viz., vacuum adsorption , dynamic adsorption, and static adsorption. The drug release differed because of three different methods. The scaffolds showed initial burst release followed by sustained drug release for period of 23 days [64].
D Huang et al have designed and developed composite scaffold support drug delivery system fabricated with an isoniazid conjugated star poly (lactide-co-glycolide) (PLGA-INH4) and β- TCP. The developed system was found to be biocompatible as indicated by cytological assay. The in vitro and in vivo drug release experiments findings showed the release of pristine INH and maintenance effective INH concentration in a controlled manner for more than 100 days. The system was able to achieve high localized drug concentration and low systemic drug concentration. Experiments in rabbits revealed bone rejuvenation and regeneration [65]. G., Wu et al have formulated an implant provided which provided prolonged and controlled drug release in the lesion. They fabricated biodegradable slow release INH/PLLA tablet using 3 dimensional printing techniques (3DP) [66]. J. Wu et al have developed rifapentine-loaded PLGA microspheres for treatment of osteoarticular TB. The microspheres were prepared by emulsion solvent evaporation method using polyvinyl alcohol as emulsion stabilizer and were evaluated for various physicchemical parameters like morphology, size distribution, and encapsulation efficiency. In vitro drug release studies were carried out in phosphate-buffered saline (PBS, 0.2 M, pH 7.4) mediums at 37.1°C. In vitro antibacterial properties of the microspheres were detected by agar diffusion test and minimal inhibitory concentration on the strains of Staphylococcus aurous (ATCC 6538) [67]. Paolino et al synthesized Bisphosphonate-polyaspartamide conjugates as potential carriers for bone targeting. Conjugates were characterized by Size exclusion chromatography and NMR. In vitro and ex vivo affinity of conjugate for bone tissue was evaluated using the hydroxyapatite and rabbit bone binding assays, respectively [68].
Intraosseous Injectable Preparation
Intraosseous infusion (IO) is the process of injecting directly into the marrow of a bone to provide a non-collapsible entry point into the systemic venous system [69]. This technique is used to provide or instill fluids and medication when intravenous access is not available or not feasible. In this the needle is injected through the bone's hard cortex and into the soft marrow interior which allows immediate access to the vascular system.
An IO infusion can be used on adult or pediatric patients when traditional methods of vascular access are difficult or impossible. In most cases, the antero-medial aspect of the upper tibia is used as it lies just under the skin and can easily be palpated and located. The anterior aspect of the femur, the superior iliac crest and the head of the humerus are other sites that can be used. Generally, any medication that can be introduced via IV can be introduced via IO. Intraosseous access has roughly the same absorption rate as IV access, and (unlike ET administration) allows for fluid resuscitation as well as high-volume drugs such as sodium bicarbonate to be administered in the setting of a cardiac arrest when IV access is unavailable. The automatic intra-osseous devices allow quick and safe access to the patient's vascular system for fluid and drug administration. There are several FDA approved IO devices: The BIG Bone Injection Gun and The NIO New Intra Osseous device are automatic intra-osseous infusion device used by military and civilian healthcare systems; the battery- powered EZ-IO and hand-powered Fast1, Fast Combat and Fast Responder. Other devices include the Cook IO needle and the Jamshidi 15G [70] (Figures 5 and 6).
Antibiotic Loaded Bone Cement
In one study Chang et al have developed bone cement comprising of antibiotics viz. Isoniazid and Rifampicin. The group formulated cement discs comprising of 1g, 2g and 4g of individual drugs and their combination. The medicated discs were evaluated for in vitro drug elution characteristics and antimycobacterial study. The result showed that Isoniazid loaded cement was found to be more effective than Rifampicin cement. Rifampicin cement was found to be ineffective because of delayed polymerization. Isoniazid cement showed antimycobacterial for 30 days. The research group suggested clinical relevance of the clinical relevance of antibiotic loaded cement that it can be employed for use in musculoskeletal tuberculosis for preventing resistance and systemic toxicity, a combination with a second-line drug [71].
Conclusion
Conventional therapy is not effective as it was earlier because of occurrence of multiple drug resistance tuberculosis, also disease advancement leads to development of kyphosis, and for its treatment advance surgery has been developed. But these techniques are not patient compliment. Thus newer methods are been developed, which will provide more target specific drug delivery in the affected area, dose reduction and shorter duration of treatments therapy. Although this is being done on very specific and selected group of patients, they could help in the near future for the treatment of bone tuberculosis. For achieving more target specific drug delivery, intraosseous injectable preparation can be formulated.
Effective amalgamation of localized chemotherapy and bone regeneration is an optimal solution to make bone TB therapy workable and successful.
Therefore, nanotechnology based formulation containing an antitubercular drug; bone replenisher is proposed to address the issue of localization and site specific delivery. The incorporation of targeting ligand mycolic acid in the carrier can help to retain the formulation at the infected site.
The bone targeted formulation will be promising approach for Tuberculosis management with less toxicity/side effects and better drug concentration at low dose.
References
- Dye C, Garnett GP, Sleeman K, Williams BG (1998) Prospects for worldwide tuberculosis control under the WHO DOTS strategy. Lancet 352: 1886-1891.
- Nakajima H (1993) Tuberculosis a global emergency. World Health 46: 3.
- Pawar UM, Kundnani V, Agashe V, Nene A (2009) Multidrug resistant tuberculosis of the spine – is it the beginning of the end? A study of twenty-five culture proven multidrug-resistant tuberculosis spine patients. Spine 34: E806-810.
- Kulchavenya E (2014) Extrapulmonary tuberculosis: are statistical reports accurate? TherAdv Infect Dis 2: 61-70.
- McClure ST (2010) What Are the Symptoms of Tuberculosis of the Bones?
- Yoon HJ, Song YG, Park WI, Chol JP, Chanh KH, et al. (2004) Clinical manifestations and diagnosis of extrapulmonary tuberculosis. Yonsei Med J 45: 453-461.
- Peto HM, Pratt RH, Harrington TA, Lobue PA, Armstrong LR (2009) Epidemiology of extrapulmonary tuberculosis in the United States, 1993-96. Clin Infect Dis 49: 1350-1357.
- Colmenero JD, Jime´nez-MejÃÆââ¬Å¾Ãâñ´as ME, Reguera JM, Palomino-Nica´s J, Ruiz-Mesa JD, et al. (2004) tuberculous vertebral osteomyelitis in the new millennium: still a diagnostic and therapeutic challenge. Eur J ClinMicrobiol Infect Dis 23: 477-483.
- Serrallach CP, Pardo DR (2013) Bone and joint tuberculosis. Eur Spine J 22: S556–S566.
- Pertuiset E, Beaudreuil J, Liote F, Horusitsky A, Kemiche F, et al. (1999) Spinal tuberculosis in adults. A study of 103 cases in developed country, 1980-1994. Medicine (Baltimore) 78: 309-320.
- Jain AK (2010) Tuberculosis of the spine. J Bone Joint Surg (Br) 92-B: 905-913.
- Kaila R, Am Malhi, Mahmood B, Saifuddin A (2009) The incidence of multiple level non-contiguous vertebral tuberculosis detected using whole spine MRI. Eur Spine J 18: 1096-1101.
- Jutte PC, Louenhout-Royackers JH, Borgdorf MW, Horn JR (2004) Increase of bone and joint tuberculosis in the Netherlands. J Bone Joint Surg 86: 901-904.
- Gardam M, Lim S (2005) Mycobacterial osteomyelitis and arthritis. Infect Dis Clin N Am 19: 819-830.
- Pigrau-Serrallach C, RodrÃÆââ¬Å¾Ãâñguez-Pardo D (2011) 20 September April 201.
- McLain RF, Isada C (2004) Spinal tuberculosis deserves a place on the radar screen. Cleve Clin J Med 71: 543-549.
- Alavi SM, Sharifi M (2010) Tuberculous spondylitis: risk factors and clinical/paraclinical aspects in the south west of Iran. J Infect Public Health 3: 196-200.
- Kaila R, Malhi AM, Mahmood B, Saifuddin A (2007) The incidence of multiple level noncontiguous vertebral tuberculosis detected using whole spine MRI. J Spinal Disord Tech 20: 78-81.
- Burrill J, Williams CJ, Bain G, Conder G, Hine AL, et al. (2007) Tuberculosis: a radiologic review. Radiographics 27: 1255-1273.
- Zhang Y (2005) The magic bullets and tuberculosis drug targets. Annu Rev PharmacolToxicol 45: 529-564.
- Mitchison DA (2004) Thesearchfornewsterilizinganti-tuberculosisdrugsFront.Biosci9: 1059-1072.
- Lenaerts AJ (2005) Preclinical testing of the nitroimidazopyran PA-824 for activity against Mycobacterium tuberculosis in a series of in vitro and in vivo models, Antimicrob.AgentsChemother49: 2294-2301.
- Medical Research Council Working Party on Tuberculosis of the Spine (1998) A 15-year assessment of controlled trials of the management of tuberculosis of the spine in KoreaandHongKong.ThirteenthReportoftheMedicalResearchCouncilWorking PartyonTuberculosisoftheSpine.JBoneJointSurgBr80:456-462.
- Alejandro Sosnik(2010)New old challenges in tuberculosis: Potentially effective nanotechnologiesindrugdelivery. AdvancedDrugDeliveryReviews62: 547-559.
- Stock D, Leslie AG, Walker JE (1999) Molecular architecture of the rotary motor in ATP synthase.Science286:1700.
- Marks Jr SC, Odgren PR (2002) Structure and development of the skeleton, in: J.P. Bilezikian , L.G. Raisz, G.A. Rodan (Eds.), Principles of Bone Biology, 2nd ed., AcademicPress,SanDiego 3-15.
- SankaranB (1993) TuberculosisofBones&Joints.IndJ Tub 40: 109.
- Manfredi R, Nanetti A, Dal Monte P, Calza L (2009) Increasing pathomorphism of pulmonarytuberculosis:Anobservationalstudyofslowclinical,microbiologicaland imagingresponseoflungtuberculosistospecifictreatment.Whichroleforlinezolid? BrazJInfectDis 13:297-303
- Falk R, Randolph TW, Meyer JD, Kelly RM, Manning MC (1997) Controlled release of ioniccompoundsfrompoly(L-lactide)microspheresproducedbyprecipitationwitha compressedantisolvent.JControlRelease 44:77-85
- Sharma SK, Mohan A (2003) Scientific basis of directly observed treatment, short-course (DOTS).JIndianMedAssoc101:157-158.
- Dheda K, Warren RM, Zumla A, Grobusch MP (2010) Extensively drug- resistant tuberculosis: Epidemiology and management challenges. Infect Dis Clin North Am2:705-725.
- SankaranB (1993) TuberculosisofBonesandJoints. IndJ Tub 40: 109.
- Suárez-García I, Noguerado A (2012) Drug treatment of multidrug-resistant osteoarticular tuberculosis:asystematicliteraturereview.IntJInfectDis 16:e774-e778.
- WHO.GlobalTuberculosisControl:Surveillance,Planning,Financing.WHOreport WHO/HTM/TB/2005.349. Geneva: WHO; 2005.
- Bruno B, Rotta M, Patriarca F (2007) A comparison of allografting with autografting for newly diagnosed myeloma. N Engl J Med 356: 1110-1120.
- https://www.orthobullets.com/basic-science/9011/bone-graftingaccessedonFebruary29,2016
- Couri C (2009)C-peptide levels and insulin independence following autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus". JAMA 301: 1573-1579.
- https://eorthopod.com/anterior-lumbar-fusion-with-cages/accessedonOctober9,2016
- Riew KD, Rhee JM (2002) The use of titanium mesh cages in the cervical spine. ClinOrthopRelatRes394: 47-54.
- MajdME,VadhvaM,HoltRT(1999)Anteriorcervicalreconstructionusingtitanium cagewithanteriorplating.Spine(PhilaPa1976)24: 1604-1610.
- Eck KR, Bridwell KH, Ungacta FF (2000) Analysis of titanium mesh cages in adultswithminimumtwo-yearfollow-up.Spine(PhilaPa1976)25: 2407-2415
- ChenY,ChenD,GuoY(2008)Subsidenceoftitaniummeshcage:astudybased on300cases.JSpinalDisssordTech21: 489-492.
- Low S, KopecÃÆââ¬Â¹Ãâââ¬Â¡ek J (2012) Targeting polymer therapeutics to bone. Adv Drug Deliv Rev64:1189-1204.
- PerrinRA (1965) BindingofTetracyclinetobone.Nature 208:787-788.
- Wang D, Miller S, Sima M., Kopeckova P, KopecÃÆââ¬Â¹Ãâââ¬Â¡ekJ (2005)Bone targeting MacromolecularTherapeutics. AdvancedDrugDeliveryReview 57:1049-1076.
- Johnsson M,Levine MJ,Nancollas GH (1993)HydroxyapatiteBindingDomainsin Salivary Proteins, Critical Reviews in Oral Biology and Medicine 4: 371-378.
- Agarwal S, Gupta A, Grevious M (2009) Use of resorbable implants for mandibular fixation:asystematicreview.JCraniofacSurg20:331-339.
- Wang(2015)Tetracycline-graftedPLGAnanoparticlesasbone-targetingdrugdelivery system,InternationalJournalofNanomedicine 10: 5671-5685.
- CaiK,YaoK,YangZ (2007)Histologicalstudyofsurfacemodifiedthreedimensional poly (D, L-lactic acid) scaffolds with chitosan in vivo. J Mater Sci Mater Med 18:2017-2024.
- Yin(2014)Asparticacid-basedmodifiedPLGA–PEGnanoparticlesforbonetargeting: Invitroandinvivoevaluation. ActaBiomaterialia10: 4583-4596.
- DingM,RøjskjaerJ,ChengL(2012)Theeffectsofanovel-reinforcedbonesubstitute andColloss_Eonbonedefecthealinginsheep.JBiomedMaterResBApplBiomater100:1826-1835
- Bose S, TarafderS (2012) Calcium phosphate ceramic systems in growth factor and drug deliveryforbonetissueengineering:areview.ActaBiomater8:1401-1421.
- HassanMA,AhmedIS,CampbellP (2012)Enhancedgenetransfectionusingcalcium phosphate co-precipitates and low-intensity pulsed ultrasound. Eur J Pharm Sci 47:768-773.
- Ronca A, Ambrosio L, Grijpma DW (2012) Design of porous three-dimensional PDLLA/nano-hap composite scaffolds using stereolithography. J ApplBiomaterFunctMater10:249-258.
- Minnikin DE (1982) Lipids: Complex Lipids, their Chemistry, Biosynthesis and Role AcademicPress,London,UK(1982).
- Dobson G, Minnikin DE, Minnikin SM, Parlett JH, Goodfellow M (1985)Magnusson MRSystematic analysis of complex mycobacterial lipids Chemical Methods of Bacterial Systematics, Academic Press, London.
- Beckman EV, PorcelliSA, Morita CT, Behar SM, Furlong ST (1994) Recognition of a lipid antigen byCD1-restricted αβ+ T cell. Nature 372: 691-694.
- Goodrum MA, Siko DGR, Niehues T, Eichelbauer D, Verschoor JA (2001)Mycolic acids from Mycobacterium tuberculosis: purification by countercurrent distribution andTcellstimulation.Microbios: 106: 55-67.
- https://www.nature.com/nrmicro/journal/v12/n8/box/nrmicro3299_BX1.html
- Lemmer Y, Kalombo L, Pietersen RD, Jones AT, Semete-Makokotlela B, et al. (2015) Mycolic acids, a promising mycobacterial ligand for targeting of nanoencapsulateddrugsintuberculosis. JournalofControlledRelease211: 94-104.
- Weber S, Zimmer A, Pardeike J (2014) Solid Lipid Nanoparticles (SLN) and NanostructuredLipidCarriers(NLC)forpulmonaryapplication:Areviewofthestate oftheart. EuropeanJournalofPharmaceuticsandBiopharmaceutics86: 7-22.
- Mehanna M, Mohyeldin S, Elgindy N (2014) Respirablenanocarriers as a promising strategyforantituberculardrugdelivery. JournalofControlledRelease187: 183-197.
- Pham D, Fattal E, Tsapis N (2015) Pulmonary drug delivery systems for tuberculosis treatment.InternationalJournalofPharmaceutics478: 517-529.
- Yuan J, Wang B, Han C, Lu X, Sun W, et al (2015)In vitro comparison of three rifampicin loading methods in a reinforced porous β-tricalcium phosphate scaffold. Journal of Materials Science: MaterialsinMedicine 26:174.
- Huang D, Li D, Wang T, Shen H, Zhao P,etal. (2015)Isoniazidconjugatedpoly (lactide-co-glycolide):Long-termcontrolled drug release and tissue regeneration for bone tuberculosis therapy. Biomaterials52: 417-425.
- Wu G (2014) Experimental study of PLLA/INH slow release implant fabricated by three dimensional printing technique and drug release characteristics in vitro. Biomed Eng 13: 97.
- Wu J, Zuo Y, Hu Y, Wang J, Li J, et al. (2015) Development and in vitro characterization of drug delivery system of rifapentine for osteoarticular tuberculosis. Drug Design, Development and Therapy 9: 1359-1366.
- Paolino D, Licciardi M, Celia C, Giammona G, Fresta M, et al. (2015) Bisphosphonate-polyaspartamide conjugates as bone targeted drug delivery systems. J Mater Chem B 3: 250-259.
- Tobias JD, Ross AK (2010) Intraosseous infusions: a review for the anesthesiologist with a focus on pediatric use, Anesthesia& Analgesia 110: 391-401.
- https://www.nejm.org/doi/full/10.1056/NEJM199005313222206.
- Chang DH, Oh T, Cho SN, Yang JH, Park KK (2013) Isoniazid Could Be Used for Antibiotic-loaded Bone Cement for Musculoskeletal Tuberculosis: An In Vitro Study, Clinical Orthopaedics and Related Research471: 2400-2406.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences